Migraine is not exclusive to adults. An estimated 10% of school-aged children in Ireland experience migraines, with the condition often under-recognised or misattributed to other issues such as stress, eyesight problems, or behavioural concerns. For community pharmacists and their teams, being able to identify symptoms, guide appropriate treatment, and advise on when to refer is crucial in reducing the impact of migraine on children’s education, quality of life, and family wellbeing.
Understanding Migraine in Children
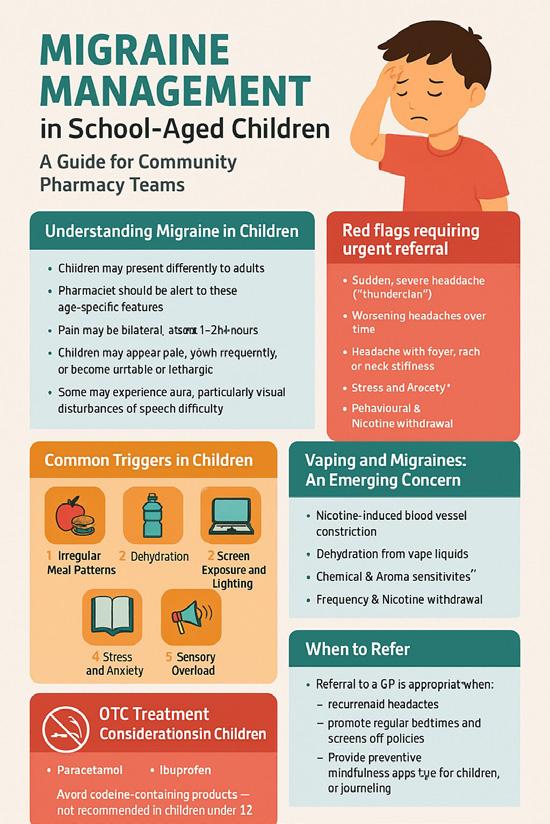
Children may present differently to adults. Pharmacists should be alert to these age-specific features:
• Pain may be bilateral rather than one-sided
• Attacks are shorter, often lasting 2–24 hours
• Children may appear pale, yawn frequently, or become irritable or lethargic
• Gastrointestinal symptoms (nausea, vomiting, abdominal pain) are more prominent
• Some may experience an aura, particularly visual disturbances or speech difficulty
Red flags requiring urgent referral include:
• Sudden, severe headache (“thunderclap”)
• Worsening headaches over time
• Headache with fever, rash, or neck stiffness
• Early morning headaches with vomiting (possible raised intracranial pressure)
• Behavioural changes or neurological signs
Pharmacy tip: Always document key features and duration of symptoms if advising OTC treatment, and clarify whether the child has a formal diagnosis.
Common Triggers in Children
The school environment presents several unique migraine triggers for children. Pharmacists should be aware of these when advising parents or young patients, especially if attacks are reported during or after school hours.
1. Irregular Meal Patterns
Busy school mornings or skipped lunches can lead to dips in blood sugar, a known migraine trigger. Encourage families to ensure children eat breakfast and have access to nutritious snacks during the day. Lunchboxes with balanced options and hydration are key.
2. Dehydration
Children may avoid drinking water during school hours to skip toilet breaks. This can lead to dehydration, especially in warmer weather or after physical education. Parents should be advised to send children with refillable water bottles and encourage regular intake.
3. Screen Exposure and Lighting
Smartboards, flickering fluorescent lights, and prolonged screen use (including tablets or phones during breaks) can act as visual triggers. Where patterns are suspected, advise parents to speak with the school about seating arrangements or lighting adjustments.
4. Stress and Anxiety
Academic pressure, tests, social challenges, or bullying may contribute to emotional stress
– a common trigger. Encourage open family communication and suggest mindfulness or relaxation techniques suitable for children.
5. Sensory Overload
Noisy classrooms, strong smells (e.g., cleaning products, markers), or crowded assemblies may overwhelm children prone to sensory sensitivity. Identifying and managing these environmental triggers can help reduce attack frequency.
Pharmacists can gently prompt: “Do the headaches tend to happen more during the school week than the weekend?” – This often uncovers a pattern.
Vaping and Migraines: An Emerging Concern
While vaping is often perceived as less harmful than smoking, growing evidence suggests it may be a trigger for frequent headaches and migraines, especially in children and teenagers.
1. Nicotine-Induced Blood Vessel Constriction
Vaping delivers nicotine, which causes vasoconstriction— narrowing of cerebral blood vessels. This mechanism is strongly linked with migraine onset in susceptible individuals.
2. Dehydration from Vape Liquids
Propylene glycol (PG) and vegetable glycerin (VG), common vape carriers, are hygroscopic (they draw moisture), increasing dehydration risk, an established migraine trigger.
3. Chemical & Aroma Sensitivities
Flavourings and sweeteners in e-liquids (e.g., sucralose, spicy or fruity scents) can provoke headaches or migraines in sensitive individuals.
4. Frequency & Nicotine Withdrawal
Daily vaping that escalates nicotine intake or sudden reduction can lead to withdrawal headaches and increased.
OTC Treatment Considerations in Children
Pharmacists and their teams should ensure that product selection and dosing are safe and age-appropriate. Treatment works best if taken at migraine onset.
First-Line Options
1. Paracetamol
o Suitable for children >2 months (ensure weight-based dosing)
o Liquid formulations for younger children
2. Ibuprofen
o More effective in some cases; avoid on empty stomach
o Suitable from 3 months (again, dose by weight)
o Avoid if dehydrated or with vomiting to reduce renal risk
Avoid codeine-containing products – not recommended in children under 12 and restricted under EU guidance.
Antiemetics
• Often prescription-only in paediatrics (e.g., domperidone, prochlorperazine)
• Pharmacists should advise parents to consult a GP if nausea or vomiting is a regular feature
Triptans
• Triptans are not generally available OTC for children in Ireland
• Some (e.g., sumatriptan nasal spray) may be prescribed for children ≥12
• Always refer children for a formal diagnosis before any triptan treatment is considered
When to Refer
Referral to a GP is appropriate when:
• The child experiences recurrent headaches affecting school or activities
• OTC medications are ineffective or overused
• There are red flag symptoms
• Preventive treatment may be needed
• A formal diagnosis of migraine is not yet made
Non-Pharmacological Advice
Community pharmacy teams can play a vital role in holistic support:
• Hydration: Encourage 6–8 glasses of water a day
• Sleep hygiene: Promote regular bedtimes and screens-off policies
• Diet: Regular meals/snacks to avoid hypoglycaemia
• Relaxation: Breathing exercises, mindfulness apps for children, or journaling
• Screen breaks: Encourage breaks during prolonged screen use
Communication Tips for Pharmacy Teams
• Use reassuring, simple language for younger children
• Engage both the child and parent in the consultation
• Ask open questions: “Can you tell me what happens before the headache starts?”
• Provide written information to take home, if possible
Final Thoughts
Migraine in children is common, yet under-recognised. As accessible healthcare professionals, community pharmacists and their teams can:
• Identify symptoms early
• Support appropriate OTC treatment
• Provide non-drug advice
• Encourage diary keeping
• Refer when necessary
By working collaboratively with parents, GPs, and schools, pharmacy teams can help reduce the burden of paediatric migraine — and support children in leading healthier, more active lives.
A European Perspective: Recent Epidemiological Insights
While migraine remains a major concern in Ireland, its burden is reflected across Europe, as highlighted in a recent large-scale survey conducted across five EU countries—France, Germany, the UK, Italy, and Spain. The 2020 National Health and Wellness Survey (NHWS), published in early 2025, offered valuable insights into the prevalence, impact, and treatment patterns of migraine across the European region.
According to the findings, migraine affects around 11.5% of the adult population across these nations, aligning closely with Irish figures. Women continue to bear a disproportionate share of the burden, with prevalence rates almost twice as high as those in men. Notably, among migraine sufferers, more than a quarter (25%) reported experiencing four or more migraine days per month. Over half experienced at least four headache days monthly, highlighting that even those not diagnosed with chronic migraine often still live with significant, recurring symptoms.
These figures reinforce what many community pharmacists already observe on the ground—migraines are common, frequently disabling, and often not managed optimally.
Perhaps more concerning is the data showing persistent underdiagnosis and inconsistent treatment. While many patients reported using analgesics, triptans, or combination therapies, only a small percentage were receiving preventive treatment—despite being eligible based on migraine frequency and severity. This gap is compounded by delays in seeking medical advice, inconsistent follow-up, and challenges in accessing specialist care, particularly in rural areas.
Primary care providers remain the main prescribers of migraine medications across Europe, but the survey findings underscore the importance of a more proactive role for community pharmacists. With pharmacists often being the first point of contact, there is a unique opportunity to screen, advise, and signpost patients appropriately— especially those with frequent or poorly controlled symptoms who may benefit from preventive therapies or specialist input.
Another insight from the survey was the high prevalence of medication overuse headaches (MOH), particularly among patients frequently self-medicating with over-the-counter pain relief. Pharmacists are ideally placed to spot patterns of overuse, offer education on proper medication intervals, and suggest safer alternatives.
Ultimately, this European-level data reinforces several key themes: migraine remains underrecognised and undertreated; many patients are managing suboptimally with OTC solutions alone; and there is a growing opportunity for pharmacy-led interventions in both identification and support.
For Irish pharmacists, these findings affirm that the challenges seen here are not isolated but part of a broader pattern across Europe. They also serve as a call to action—encouraging more structured migraine consultations at the counter, better documentation of headache patterns, and proactive collaboration with GPs when red flags arise or preventive treatment may be warranted.
For further resources, both pharmacists and patients can access information and support via the Migraine Association of Ireland at migraine.ie.
Written by John McCourt, Superintendent Pharmacist, Millmount Pharmacy
Read the latest News at IPN HERE
Read IPN July HERE









